What is Dyspraxia?
Dyspraxia, also known as developmental coordination disorder (DCD) and developmental dyspraxia, is a neurological difference that usually begins manifesting during early childhood and a person’s school-age years. It affects a person’s ability to coordinate, plan and carry out physical movements. It’s not related to muscle weakness or intelligence, but rather how the brain processes information to coordinate movement. Dyspraxic people often experience:

Motor difficulties
Poor coordination and balance
Difficulty with fine motor skills, such as handwriting, using cutlery, or buttoning clothes
Difficulties with gross motor skills, like running, jumping, or catching a ball
Difficulty with planning and sequencing actions (motor planning)
Speech, perception, and memory challenges
Low self-esteem and frustration, especially in social or school settings
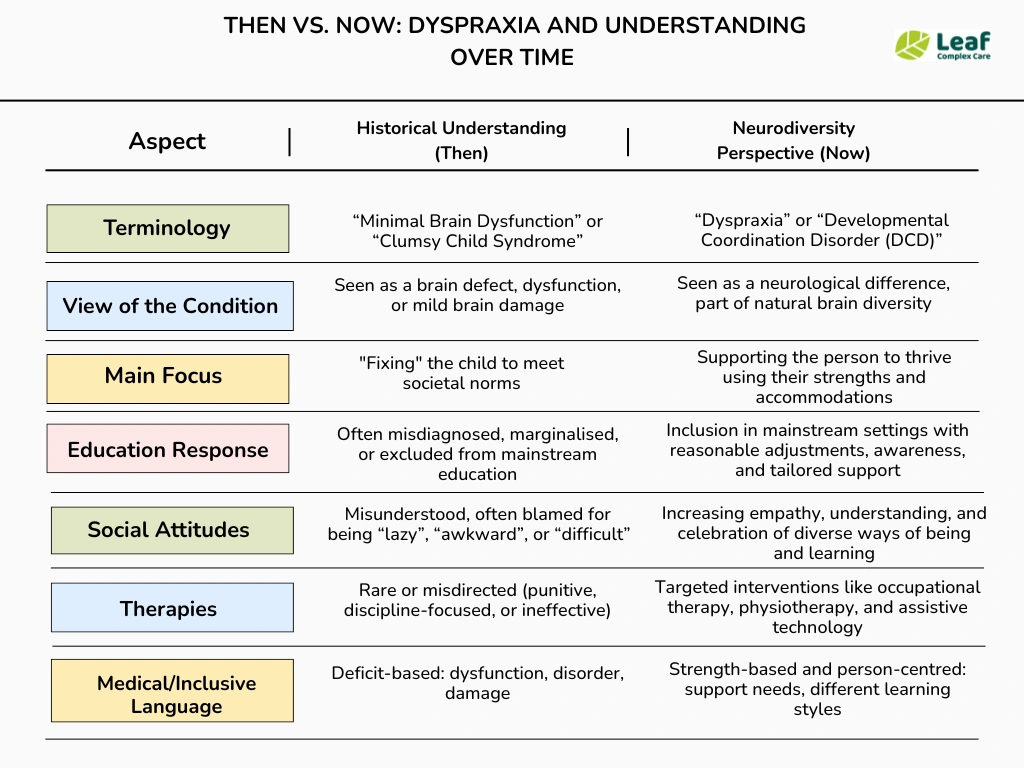
In the past, dyspraxia was poorly understood. Children struggling with coordination were often mislabelled as lazy, unintelligent, or clumsy. At one point, children who showed signs of poor coordination were commonly described as having ‘clumsy child syndrome’. In the mid-20th century, particularly in the 1960s and 1970s, some children with dyspraxia-like symptoms were labelled with “Minimal Brain Dysfunction” (MBD) – a broad and outdated term. These terms only bring stigmatisation; they are misleading and unhelpful when it comes to providing support, and only support the historical approaches where children were physically punished and totally neglected.
Today, through the lens of neurodiversity, it is acknowledged as a valid and valuable part of human variation.
How Common is Dyspraxia?
In the UK, around 5-6% of children are estimated to have dyspraxia, more commonly identified in boys. In every classroom of 30 children, approximately 1 to 2 may have dyspraxia. Many continue to experience difficulties into adulthood, but adult assessment is far less frequent due to a lack of awareness.
💡DID YOU KNOW?
- Many people live with undiagnosed dyspraxia well into adulthood.
- Dyspraxia often co-occurs with ADHD, Autism, Dyslexia, Sensory Processing Differences and learning disabilities.
Is Dyspraxia Neurodivergent?
Yes, dyspraxia is considered a form of neurodivergence.
Neurodivergence is an umbrella term that refers to variations in the brain’s wiring and functioning compared to what is considered “neurotypical.” This includes conditions like autism, ADHD, dyslexia, and dyspraxia, among others.
Dyspraxia, also known as Developmental Coordination Disorder (DCD), affects motor coordination and planning, thus impacting essential motor function in everyday tasks. Because it involves differences in neurological development and functioning, it fits within the broader neurodiversity framework that recognises and values brain differences rather than viewing them as disorders to be “fixed.”
Dyspraxia in Adults
While the effects of DCD are commonly associated with childhood, some children don’t outgrow this neurodevelopmental disorder, and many adults get diagnosed later in life. Adults with dyspraxia may also experience memory, organisation, executive functioning difficulties, and sometimes cognitive or emotional difficulties, including difficulty learning new skill .
How does dyspraxia affect adult life? People may experience many challenges work-related (challenges with manual tasks, organisation, or rime management), in their daily living (cooking, cleaning, or driving can be harder), in social situations (difficulty with physical coordination or speech can affect confidence and social engagement) and in their mental health (stress, anxiety, or depression).
Dyspraxia in Children
Dyspraxia is more detectable in early childhood because it can cause an obvious delay in the development of basic motor skills, impede language acquisition, and affect the child’s speech.
Dyspraxia in children can affect perception, not just motor skills. No two children with dyspraxia are the same; it can range from mild coordination issues to severe difficulties affecting daily functioning. Some children with dyspraxia have exceptional creativity, problem-solving abilities, or strong verbal skills, highlighting the diversity within neurodivergence.
When it comes to learning and social life, children can experience writing difficulties, specific learning difficulties and may feel ”different” which can impact their emotional well-being.
Types of Dyspraxia
Dyspraxia is commonly divided into the following types:
Motor Dyspraxia causes difficulties in everyday tasks that include precise movements, such as dressing, riding a bicycle, handwriting, and touch typing skills.
Verbal Dyspraxia, also known as developmental articulatory dyspraxia, impacts the motor neurons that control physical movements involved in speaking.
Oral Dyspraxia weakens the person’s voluntary control over movements of the lips, tongue, jaw, and soft palate.
Signs and Symptoms of Dyspraxia
Dyspraxia primarily impacts motor coordination and planning, but its effects can be wide-ranging, influencing everything from everyday physical tasks to speech and organisation. Because symptoms can vary significantly from person to person and across ages, being aware of the common indicators helps parents, educators, and caregivers identify challenges early and seek appropriate support.
Dyspraxia also comes with speech and language struggles that can influence social life, such as difficulty keeping up with conversations and responding to questions after a long pause.
Symptoms of Dyspraxia in Adults
Adults with developmental coordination disorder experience the following symptoms:
- Poor time management and organizational skills – struggles with deadlines and punctuality in the workplace
- Trouble handling essential manual tools and equipment (such as opening jars or tins)
- Difficulty learning new skills or applying them to motor tasks in a new, more dynamic environment
- Struggles with keeping balance and maintaining energy levels throughout a busy day
- Making long pauses before responding to a comment or answering a question
- Social anxiety, low self-esteem, and an avoidant approach to social situations that may expose the previously mentioned difficulties
- Academic and professional underachievement
Symptoms of Dyspraxia in Children
Children with dyspraxia show different signs and symptoms throughout different childhood stages. Developmental coordination disorder (DCD) can affect a child’s performance of routine tasks and early acquisition of motor skills.
Common signs of this motor disorder in children include:
- Delay in the earliest developmental milestones linked to movement, such as sitting, crawling, standing, walking
- Difficulty with fine motor skills, which causes slower and more hesitant movements compared to other children
- Lack of interest in movement games and activities, such as jumping, running, catching or throwing objects
- Issues with handwriting – slow writing
- Struggles with common motor performance, such as using cutlery or getting dressed
- Difficulty grasping spatial concepts (on/under/in front of/behind)
- Difficulty staying focused, indiscriminate reaction to all stimuli
- Poor balance and posture
- Speech and language delays
- Difficulty with sequencing
- Low muscle tone
- Avoidance of playing sports
- Performing physical tasks
Causes of Dyspraxia
Although the exact causes are not fully understood, research suggests that dyspraxia, unlike conditions such as cerebral palsy, results from atypical development or functioning in the parts of the brain responsible for planning, coordinating, and executing movements, particularly areas like the cerebellum and parietal lobes.
Several factors may contribute to the development of dyspraxia, including:
- Premature birth or low birth weight
- Genetic influences (having a family history of movement difficulties)
- Brain damage due to an illness, injury, or stroke
- Environmental factors

Is Dyspraxia Hereditary?
Yes, dyspraxia can have a hereditary component.
While the exact causes of dyspraxia are still being researched, studies show that it often runs in families, suggesting a genetic link. Children with a family history of dyspraxia or other neurodevelopmental conditions (like ADHD or autism) are more likely to have dyspraxia themselves. However, it’s not caused by a single gene but likely involves multiple genes interacting with environmental factors.
Dyspraxia Assessment
Assessing dyspraxia involves a comprehensive evaluation using a screening instrument to understand a person’s motor coordination difficulties and how these affect daily life. Early and accurate assessment by an occupational therapist is essential to identify needs and create an effective support plan.
Occupational therapists are usually the primary professionals involved in assessing dyspraxia. Other specialists may include physiotherapists, speech and language therapists, paediatricians, neurologists, psychologists, and speech and language therapists, depending on the symptoms and age of the person.
💡Why Is Assessment Important?
- Provides clarity on the challenges faced.
Helps rule out other conditions or identify co-existing issues.
Informs personalised therapy and support plans.
Supports access to educational accommodations and workplace adjustments.
Support for Dyspraxia
While dyspraxia is a lifelong neurological condition, many individuals can significantly improve their skills and quality of life with the proper support. Support focuses on helping people develop motor coordination, daily living skills, confidence, and self-careself-care while managing any emotional or social challenges.
Perceptual Motor Training
Perceptual motor skills involve the ability to process sensory input (such as sight, sound, and touch) and translate it into coordinated physical movement. Perceptual Motor Training exercises aim to strengthen this sensory-motor integration through structured activities that improve:
Balance and posture
Hand-eye coordination
Spatial awareness and body awareness
Motor planning and sequencing
It enhances sensory processing, builds motor coordination, improves confidence and independence, and supports academic and daily activities.
Occupational Therapy
OT is often the cornerstone of dyspraxia support, encouraging physical activity as part of the therapy . Therapists work with dyspraxic people to improve fine motor skills (like writing, using utensils), gross motor skills (like balance and coordination), and practical daily tasks (dressing, personal care). They also provide strategies to manage fatigue and sensory sensitivities.
⇒ Read more about how our occupational therapists can support you.
Physical Therapy
Physical therapists help with strengthening muscles, improving balance, posture, and overall physical coordination, which can make everyday movements easier and safer. Physical therapy is often used alongside occupational therapy and speech therapy to provide a holistic approach to managing dyspraxia, addressing fine motor skills, communication, and physical coordination together.
Speech and Language Therapy
Speech and language therapy (SLT) plays a vital role in supporting individuals with dyspraxia, especially when the condition affects oral motor skills, speech clarity, and communication. Speech and language therapy helps address these challenges by targeting:
Articulation
Oral motor control
Planning and sequencing of speech movements
Language skills
Alternative communication
⇒ Learn more about speech and language therapy.
Cognitive Behavioural Therapy
While dyspraxia is considered a lifelong condition that primarily affects motor coordination, it can also lead to emotional and psychological challenges, such as anxiety, low self-esteem, frustration, and social difficulties. This is where Cognitive Behavioural Therapy (CBT) can be a valuable support strategy. CBT helps in:
Managing anxiety and stress
Building self-esteem and confidence
Frustration and emotional regulation
Improving problem-solving and organisation
Reducing social anxiety and enhancing social skills
Dyspraxia Related Conditions
Dyspraxia rarely occurs in isolation. It is often accompanied by other neurodevelopmental or sensory conditions that can influence the experiences and challenges faced by people.
Dyspraxia and Dyslexia
Dyspraxia often occurs alongside dyslexia. According to research from the Dyspraxia Foundation, around half of the dyslexic people also have DCD. Both dyspraxia and dyslexia affect a person’s learning style, especially in the area of language acquisition. While dyslexia causes trouble connecting letters to sounds, dyspraxia impacts writing in a manual way (weak pencil grip).
Dyspraxia and ADHD
Both dyspraxia and ADHD (attention deficit hyperactivity disorder) can affect children’s educational progress and prevent them from achieving their full potential. In many cases, children with ADHD and dyspraxia may face similar challenges in the classroom, such as messy handwriting or poor posture.
What distinguishes the two conditions is the complex process behind these signs. In children with ADHD, these difficulties occur due to hyperactivity and attention issues, whereas children with dyspraxia experience them as a result of neuromotor differences.
Dyspraxia and Autism
There’s a significant overlap between the symptoms of autism and dyspraxia, especially when it comes to early signs in babies and toddlers. Both conditions may cause a delay in the earliest developmental milestones, such as sitting, crawling, walking and potty training.
As autism is a more researched and common disorder, many children with dyspraxia may get misdiagnosed. Therefore, it is important to note that dyspraxia primarily impacts movement, while autism affects social and communication skills.
Support with Leaf Complex Care
At Leaf Complex Care, we understand that every individual’s needs are unique, especially regarding conditions like dyspraxia and other neurodivergent differences. Our dedicated team works collaboratively to provide personalised, compassionate support that empowers people to live fulfilling lives with confidence and independence.
Our approach is rooted in Positive Behavioural Support (PBS), and our occupational therapists, through holistic care, ensure that all aspects of wellbeing are addressed. We offer a sensory-friendly environment, innovative therapies, and a skilled Rapid Response Service that responds promptly to changing needs. We work closely with families, professionals, and communities to create a network of support that truly makes a difference.
Download the case studies and see how our person-centred care brings positive change and empowers individuals to be as independent as possible in the community and their own homes.
If you require support, please make a referral here.
Offices: Bristol, South East, the Midlands and Somerset.

