Getting the Right Support in Place: Communication Care Plans That Work
-Blog Series with our Speech and Language Therapist, Jodee Simpson-
About Jodee:
HCPC registered Speech and Language Therapist and a certified member of the Royal College of Speech and Language Therapists.
Jodee’s Expertise:
Specialising in Eating, Drinking & Swallowing, Learning Disabilities and Autism.
Advocacy:
Keynote Speaker, Guest Lecturer, Author, and Co-founder of the UK’s first peer support network for neurodivergent speech and language therapists.
Providing effective training for care coordinators is a crucial element when it comes to providing the right care, as they constantly communicate with the support workers. With over 600 clinicians across the organisation and limited time to meet them all individually, Jodee focuses on equipping care coordinators to bridge the gap in ensuring that communication strategies are effectively implemented on a broader scale.
This approach allows the care coordinators to act as mediators, improving communication outcomes and the overall quality of care.
Jodee shares: ‘’Our care coordinators are responsible for creating communication care plans for everyone we support. The communication care plan should basically explain what that person needs to communicate at their best.”
“This includes the additional communication support they need to understand information, follow their routines, express their views, and make choices. It helps them to participate in making important decisions about their care and treatment, such as where they will live or how they want to be supported. A good communication care plan essentially identifies opportunities for the person to have more autonomy and control over their own lives by describing the communication tools that make that possible’’
Empowering Care Coordinators
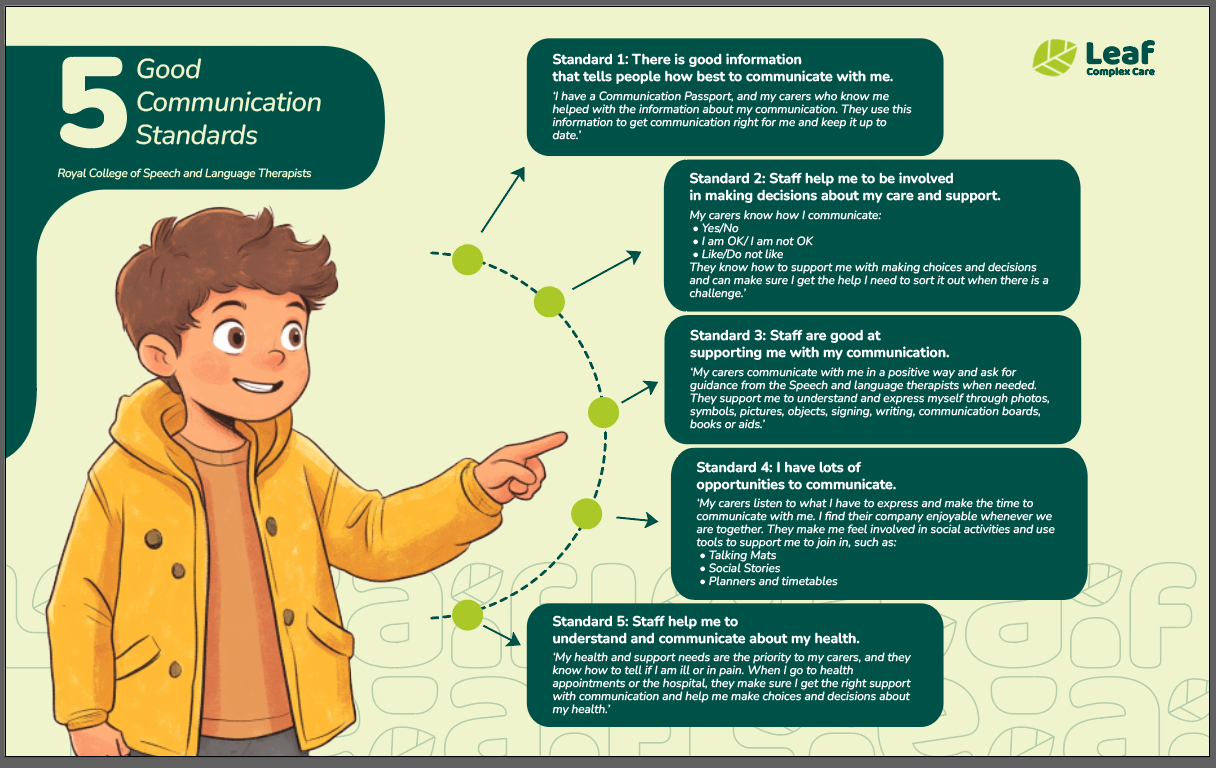
Jodee’s goal is to improve the quality of care plans through the training. She follows the guidelines set out by the Royal College of Speech and Language Therapists, known as the Five Good Communication Standards. Communication profiles are an essential part of understanding how to support people in the right way.
“Care coordinators are the bridge between support workers and those we support. They pull together care plans, ensure they’re implemented, and adapt them as needed. Training care coordinators was a natural step to improve communication outcomes across the organisation.
Through targeted training sessions, I’ve seen remarkable transformations. For instance, one coordinator shared how understanding a person’s preference for non-speaking cues like gestures and rhythms changed how they approached care. This shift enhanced communication and deepened trust and the emotional bonds between the person and their care team.”
Care coordinators are central to the success of communication care plans. Their role as mediators ensures that individuals’ voices are heard while supporting clinicians in implementing plans.
‘’My thoughts were that I wanted to introduce the care planning training because I thought, actually, if we get the care plan right, then we can get the care right because the clinicians are following a care plan.
We support people to actively engage in making decisions about their care and support. It’s about involving people, but more importantly, getting the communication right to support them. To achieve that standard, staff use communication tools that we, as speech and language therapists, thoughtfully create. We pull it together and make the resources so it’s there to help that person. And it often reduces their anxiety.’’
We've put together a communication plan template that you can use if you're involved in someone's care or support.
Supporting People Who Have Minimal Speech
Supporting people who are non-speaking or with few recognisable words need a lot of support from their communication partners to create opportunities for them to engage with other people and participate in making simple everyday choices.
“I often see this when people say, ‘Well, I know they only ever want a cup of tea, so it doesn’t matter. If I ask them what they want to drink, they’re always going to say a cup of tea. So now, I don’t bother asking them. I just make them a cup of tea.’ But this approach takes away the person’s opportunity to make a choice. What if, one day, they change their mind and decide they want orange juice? By not asking, they lose the chance to change their mind and express themselves, even in small ways. For people with a learning disability, this is particularly significant because, for some, those small expressions might be the only words they can use—like ‘tea’ or ‘toilet. It’s vital to provide plenty of opportunities for people to keep their language skills active, even if it means having the same conversation repeatedly. Saying ‘yes’ or ‘no’ empowers them to make decisions.

‘’And this principle extends to health-related scenarios. For instance, if someone needs to attend an appointment or undergo a procedure, we don’t simply take them without preparation. We ensure they understand what’s happening, reducing distress by involving them in the process. These practices embody the essence of the five good communication standards, which is the basis of what speech and language therapy is all about.”
And why is the right communication plan and support is so essential? Jodee shares:
‘’I’ve asked the care coordinators to rate how they feel about various aspects of communication, as these are often areas we include in a person’s communication care plan. For example, What does that person need to help them understand? How do we support them in expressing their views and wishes? How do we enable them to make choices? These questions guide us, but there are also critical elements to consider, like recognising how someone feels and fostering a relationship with them. This is crucial because people need to feel safe. Many of those we work with have experienced significant trauma, failed placements, or faced distressing circumstances. Some have even had mental health admissions, which can be incredibly traumatic, leaving them feeling unsafe.
Supporting people in the community requires us to prioritise relationship-building as a fundamental part of our care. When someone feels understood and secure, it lays the groundwork for meaningful communication and progress in their overall well-being.“
Supporting Everyday Communication in Care Through A Practical Approach
In Jodee’s training sessions, communication support is divided into three main areas: everyday communication, building positive relationships and spotting how someone is feeling. This approach empowers people, reduces distress and fosters independence.
Let Jodee walk you through this concept using real-life examples from her experience.
“In the training, I split communication into three areas. Everyday communication is about helping people understand. It’s about asking, ‘What does that person need to understand everyday things?’ For example, do they know what ‘It’s time to brush your teeth’ means? Or do they need a picture to help them understand what’s next in their routine?’’
Many people need prompts to guide them, but not all prompts have to be verbal. For instance: “Can we give people prompts without actually having to use words? Can we use a picture prompt or a schedule if they don’t use words? For example, a schedule could say, ‘First brush teeth, then wash face, then sit on the toilet.’ With this, they can follow the steps themselves, promoting independence.”
Tools to Enhance Understanding in Communication Care Planning
Various tools can be introduced to help people comprehend and engage with their routines.
“Speech and language therapy often helps determine how much someone understands. From this, we can advise on tailored strategies—like using picture cards, gestures, or even communication aids like iPads. These tools can ensure everyone is on the same page.”
Some people who are non-speaking can still communicate effectively through choices.
“For example, I’ve worked with people who use communication books filled with pictures of their options for the day. They can go through these and choose, saying, ‘Let’s do that one today.’ This way, they stay in control, even without using speech.”
Consistency and clarity in routines can alleviate much of the anxiety people feel about the unknown. Tools like visual timetables or “Now and Next” boards can be invaluable.
“Some people can only cope with immediate tasks, so we use what’s called a ‘Now and Next’ board. This shows what’s happening now and what’s coming next. For others, a timetable for the day—or even the week—can be helpful. It all depends on what they can process. These strategies help reduce uncertainty, creating a more predictable environment that encourages calm and focus.
When people know what’s happening next, they’re less anxious. They feel more secure and better able to participate.”
Recognising Demand Avoidance and Reducing Distress
Some people experience significant anxiety when given direct verbal instructions, a condition often referred to as demand avoidance. For them, constant verbal prompting can feel overwhelming.
“For some people we support, being told what to do can feel like nagging. It’s the equivalent of someone saying, ‘Do this, do this, do this!’ repeatedly. This can lead to distress and refusal.”
For these cases, non-speaking methods can make a substantial difference.
“Sometimes, finding ways that aren’t verbal can help reduce demands. For instance, using Makaton signing, showing pictures, or slowing down and giving one instruction at a time. For someone who can only process one thing at a time, you might say just one word, like ‘Coat,’ while using a gesture to indicate putting it on.”
Closing Thoughts
Supporting everyday communication is about meeting people where they are and giving them the tools to thrive. With careful attention and the right resources, we can create environments where everyone can feel seen, heard, and valued.
What We Recommend Reading:
The Language of Difference: Understanding Autistic Communication Differences – the first blog post co-written with Jodee Simpson, Speech and Language Therapist at Leaf Complex Care, and across the Catalyst Care Group’s organisations.
Stick around for our monthly blog series, with first-hand information on approaches and practices our specialists employ when supporting people in complex situations, with multiple needs.
Explore our multidisciplinary team’s expertise and get the support you require!

