What Is Trauma-Informed Care?
Trauma-informed care (TIC) is a whole-system approach that recognises common traumatic experiences, understands their effects on health and behaviour, and reshapes services. Hence, they do no further harm, promote safety and trust, and support recovery. Trauma is common and can shape physical and mental health across the life course (links to PTSD, substance misuse, and long-term conditions). This approach seeks to avoid re-traumatisation by building consistent, trusting relationships and safe environments.
Care that ignores trauma risks harm. Services that don’t recognise trauma can inadvertently retraumatise people (for example, by using coercive practices or not explaining procedures). Trauma-informed approaches aim to prevent that harm.
What Trauma-informed Care is Not
Trauma-informed care is not a single psychological therapy. It is an approach to how services operate (although trauma-focused therapies are part of clinical pathways for PTSD). SCIE and local authorities emphasise trauma-informed practice for adults with learning disabilities and autistic adults who have experienced trauma exposure, including trauma-specific services.

Awareness of the Prevalence of Trauma
The starting point of trauma-informed care is the awareness of the prevalence of trauma. According to Public Health England’s report on Adverse Childhood Experiences (ACEs), around half of adults in England and Wales have experienced at least one form of trauma during childhood, such as abuse, neglect, domestic violence, or living with someone who misused substances or had mental health difficulties. A significant proportion have experienced multiple ACEs, which increases the likelihood of physical and psychological difficulties later in life.
The Substance Abuse and Mental Health Services Administration (SAMHSA) further highlights that trauma is not only individual but can also be collective and intergenerational. This “historical trauma” refers to the cumulative emotional and psychological wounding passed down through generations after large-scale group trauma, such as oppression, forced displacement, or discrimination, and continues to influence mental and physical health outcomes, behaviour, and trust in services today.
This awareness shifts professional practice from asking “What’s wrong with you?” to “What’s happened to you?”
Let’s see the data:
- 47% of adults in England report at least one ACE.
- 9% report four or more ACEs, putting them at higher risk of mental health conditions, substance use, and long-term physical illnesses.
- 1 in 4 women and 1 in 6 men in the UK experience domestic abuse in their lifetime.
- An estimated 3.1 million adults in England and Wales have experienced sexual assault or attempted assault since the age of 16.
Acknowledging how widespread trauma is, UK health, social care, and trauma-informed organisations move from isolated therapeutic responses to systemic compassion and cultural change.
Re-Traumatisation
Re-traumatisation occurs when an individual is exposed to situations, environments, or interactions that trigger memories or feelings associated with past trauma, causing them to re-experience the emotional or physiological distress of the original event, which can have a negative impact. In health and social care, re-traumatisation can happen unintentionally, often through well-meaning but poorly informed practices, environments, or communication styles. The Substance Abuse and Mental Health Services Administration (SAMHSA) points out that re-traumatisation can occur through “seemingly neutral policies and practices” that replicate the dynamics of past trauma. Examples include rigid rules, lack of voice or choice, or environments that remind people of previous power imbalances.
To reduce the risk of re-traumatisation, mental health services should embed trauma-informed care at every level of support. This includes:
- Providing supportive and compassionate responses to trauma histories
- Explaining processes clearly, seeking consent at every stage, and honouring the person’s right to decline or ask questions.
- Encouraging people to make decisions about their care, including where and how support is provided.
- Maintaining emotional safety by using a non-judgmental approach
- Assessing and focusing on people’s strengths
- Providing a safe and comfortable environment
- Recognising how stress can show up suddenly and help regulate their response
A Trauma-Informed Approach
The trauma-informed approach transforms organisations from systems that may unintentionally replicate harm to ones that actively support healing and resilience. It is a cultural and organisational framework designed to ensure that all interactions, policies, and environments prioritise the trauma-informed principles.
The trauma-informed model is being guided by the “Four Rs”:
- Realise the widespread impact of trauma and understand paths for recovery.
- Recognise the signs and symptoms of trauma in supported people, families, staff, and others involved.
- Respond by integrating knowledge about trauma into policies, procedures, and practices.
- Resist Re-traumatisation by creating safe, supportive, and encouraging environments.
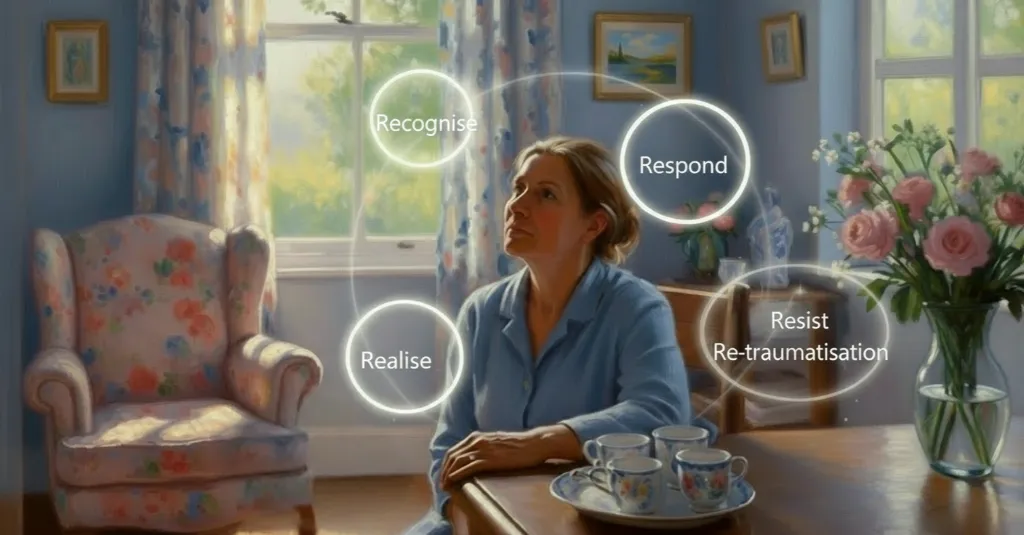
These “Four Rs“ ensure that trauma-informed care is preventative and restorative, avoiding harm while actively fostering resilience and recovery.
Read more about how is trauma-informed care integrated in Speech and Language therapy.
Key Principles of Trauma-Informed Care
A trauma-informed care approach is built on a set of core principles that shape how organisations understand, respond to, and support individuals affected by trauma. These principles provide a foundation for creating safe, compassionate, and empowering services for the people receiving care and the staff providing it.
Let us walk you through the six core principles of trauma-informed care:
Safety
Safety is the soil from which healing grows. It transforms care from being procedural to being relational, where every interaction, environment, and policy communicates:
“You are safe here. You will be treated with dignity, and your experience matters.”
People have to feel safe when others care for them. For example, medical professionals should ensure that people who have gone through a traumatic event and their families feel physically and emotionally safe while in their care. Care teams should establish safe settings that are calm and predictable, the care is consistent and respectful, and people are always informed about what is happening and why.
Trustworthiness
Trauma can erode a person’s ability to trust others. Building trust requires openness, honesty, and consistency. Organisations should make decisions in clear and transparent ways, explaining processes and respecting confidentiality. Transparency in communication, for example, being upfront about what services can and cannot do, helps people regain control and stability.
Also, healthcare professionals should always be transparent about policies and procedures that might impact how people who have experienced trauma react.
Collaboration
Trauma-informed care acknowledges that recovery is most effective when relationships are based on partnership rather than hierarchy. Collaboration reduces power imbalances between professionals and the people they support. NICE guidance encourages practitioners to involve people and families in decision-making and planning, fostering shared ownership of goals and outcomes.
According to the NHS’s Guidance for Integrated Care Systems to deliver Trauma Informed Mental Health Transformation (2022), collaboration means “working alongside people, valuing their lived experience, and co-producing care in a way that recognises shared humanity.” Professionals are encouraged to approach each interaction as a two-way relationship, where the practitioner and the person bring valuable knowledge. The professional contributes technical expertise, and the person contributes lived experience and insight into what helps them feel safe and supported.
Empowerment
Support workers need to empower individuals who have experienced trauma to help them regain control of their health. To do this, they often share their stories and show that they are easy to communicate with. Effective communication is crucial when getting to know someone and allowing them to learn more about you and trust you. A trauma-informed practice promotes a system that helps people to communicate and grow from trauma.
Practical еxamples:
- A social worker offering multiple options for therapy modalities and allowing the client to choose.
- Allowing residents to set their daily routines or participate in menu planning.
- Involving people in staff recruitment panels or feedback forums to influence organisational decisions.
- Educational settings providing students with flexible ways to complete work that respect their needs and preferences.
Peer Support
Peer support involves mutual, non-hierarchical relationships where individuals who have experienced trauma provide guidance, encouragement, and understanding to others facing similar challenges. It is based on the idea that lived experience creates a level of empathy and credibility that professionals without those experiences may find difficult to match.
Key aspects include:
- Community building: Encouraging connection and reducing social isolation by linking individuals with supportive networks.
- Emotional support: Offering understanding, validation, and empathy through shared experiences.
- Practical guidance: Sharing coping strategies, navigating services, and problem-solving.
- Role modelling recovery: Demonstrating that healing is possible, which fosters hope and motivation.
Cultural, Historical, and Gender Awareness
This principle recognises that trauma does not occur in a vacuum, and that it is often shaped by social, cultural, historical, and systemic factors. Trauma-informed care acknowledges cultural aspects (such as language, communication styles, beliefs about health, wellbeing, and healing practices), historical experiences (including discrimination against ethnic minority communities) and gender-related factors (such as domestic abuse or sexual violence, among women, men, and non-binary people) all influence how trauma is experienced. Trauma-informed care recognises the broader context of a person’s experiences, supporting healing more holistically and sensitively.
Practical Implementation:
- Include cultural competence training for all staff.
- Incorporate trauma history that considers historical and intergenerational factors into assessments.
- Design services that are accessible, inclusive, and sensitive to gender-specific experiences.
- Co-produce policies and programmes with diverse communities to ensure relevance and safety.
Goals of Trauma Informed Care
The overarching goal of trauma-informed care is to shift the culture of services from reactive to proactive, from punitive or deficit-focused to empathetic, empowering, and healing-oriented. It ensures that every level of an organisation, from leadership to frontline staff, actively contributes to creating an environment that respects, understands, and supports people who have experienced trauma.
When fully embedded, trauma-informed care moves systems from reactive, fragmented responses to compassionate, strengths-based, and inclusive practices, ensuring that every person is treated with dignity, respect, and understanding.
About Leaf Complex Care
Leaf Complex Care is a social care provider that supports young people and adults in complex situations with multiple needs, primarily autistic and with/or without a learning disability.
We are officially Autism Accredited for our support, meaning our services offer:
- More autism-focused support
- More personalised approaches, always putting the supported person and their families at the centre of care decision-making.
- Increased expertise in supporting autistic people and providing better outcomes
- Reassurance for families/carers
The foundation of our humanised support lies in our highly trained support workers and expert therapy team, who set the goals for support by placing the person’s needs and wants at the centre of care.
Our specialists use:
- Person-centred approach to care
- Autism-informed approach
- Trauma-informed approach
- Relationship-based practices
- Outcome-focused approach
- The Capable Environment Model of Support
- The PERMA Model of Wellbeing
- The PACE Model of Support
We provide local support in the areas of Bristol, the South East, the Midlands, and Somerset.

